Search
- Page Path
- HOME > Search
- Miscellaneous
- Corrigendum: Correction of Acknowledgments. Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
- Endocrinol Metab. 2022;37(1):180. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.103
- Corrects: Endocrinol Metab 2021;36(4):717
- 2,571 View
- 107 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Lateral Involvement in Different Sized Papillary Thyroid Carcinomas Patients with Central Lymph Node Metastasis: A Multi-Center Analysis
Yu Heng, Zheyu Yang, Pengyu Cao, Xi Cheng, Lei Tao
Journal of Clinical Medicine.2022; 11(17): 4975. CrossRef
- Lateral Involvement in Different Sized Papillary Thyroid Carcinomas Patients with Central Lymph Node Metastasis: A Multi-Center Analysis

- Thyroid
- Clinical Characteristics and Prognosis of Coexisting Thyroid Cancer in Patients with Graves’ Disease: A Retrospective Multicenter Study
- Jee Hee Yoon, Meihua Jin, Mijin Kim, A Ram Hong, Hee Kyung Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(6):1268-1276. Published online November 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1227
- 4,837 View
- 186 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The association between Graves’ disease (GD) and co-existing thyroid cancer is still controversial and most of the previously reported data have been based on surgically treated GD patients. This study investigated the clinicopathological findings and prognosis of concomitant thyroid cancer in GD patients in the era of widespread application of ultrasonography.
Methods
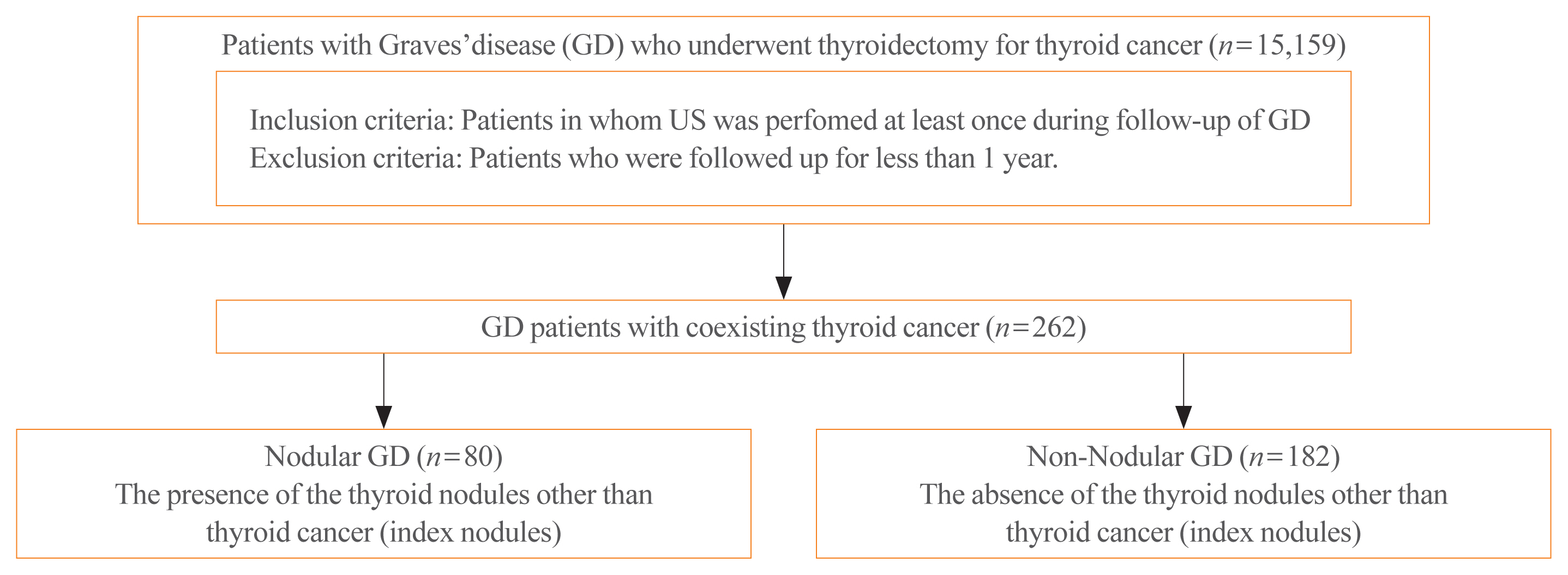
Data of GD patients who underwent thyroidectomy for thyroid cancer between 2010 and 2019 in three tertiary hospitals in South Korea (Asan Medical Center, Chonnam National University Hwasun Hospital, and Pusan National University Hospital) were collected and analyzed retrospectively. In the subgroup analysis, aggressiveness and clinical outcomes of thyroid cancer were compared nodular GD and non-nodular GD groups according to the presence or absence of the thyroid nodules other than thyroid cancer (index nodules).
Results
Of the 15,159 GD patients treated at the hospitals during the study period, 262 (1.7%) underwent thyroidectomy for coexisting thyroid cancer. Eleven patients (4.2%) were diagnosed with occult thyroid cancer and 182 patients (69.5%) had microcarcinomas. No differences in thyroid cancer aggressiveness, ultrasonographic findings, or prognosis were observed between the nodular GD and non-nodular GD groups except the cancer subtype. In the multivariate analysis, only lymph node (LN) metastasis was an independent prognostic factor for recurrent/persistent disease of thyroid cancer arising in GD (P=0.020).
Conclusion
The prevalence of concomitant thyroid cancer in GD patients was considerably lower than in previous reports. The clinical outcomes of thyroid cancer in GD patients were also excellent but, more cautious follow-up is necessary for patients with LN metastasis in the same way as for thyroid cancer in non-GD patients. -
Citations
Citations to this article as recorded by- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease
Suo-Hsien Wang, Wu-Po Chao, Ta-You Lo, Soh-Ching Ng, Yu-Hsien Chen
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2024; 34(2): 150. CrossRef - Outcomes of Surgical Treatment for Graves’ Disease: A Single-Center Experience of 216 Cases
Hanxing Sun, Hui Tong, Xiaohui Shen, Haoji Gao, Jie Kuang, Xi Chen, Qinyu Li, Weihua Qiu, Zhuoran Liu, Jiqi Yan
Journal of Clinical Medicine.2023; 12(4): 1308. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Risk and Prognosis of Thyroid Cancer in Patients with Graves’ Disease: An Umbrella Review
Marco Palella, Francesca Maria Giustolisi, Adriana Modica Fiascaro, Martina Fichera, Antonella Palmieri, Rossella Cannarella, Aldo E. Calogero, Margherita Ferrante, Maria Fiore
Cancers.2023; 15(10): 2724. CrossRef - Characteristics, staging and outcomes of differentiated thyroid cancer in patients with and without Graves’ disease
Chaitra Gopinath, Hanna Crow, Sujata Panthi, Leonidas Bantis, Kenneth D. Burman, Chitra Choudhary
Journal of Clinical & Translational Endocrinology.2023; 33: 100321. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Hashimoto’s Thyroiditis and Papillary Thyroid Carcinoma: A Follow-Up Study in Patients with Absence of Aggressive Risk Factors at the Surgery of the Primary Tumor
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Sonia Vargiu, Angela Spanu, Giuseppe Madeddu
Diagnostics.2023; 13(19): 3068. CrossRef - Table of Contents
Clinical Thyroidology.2022; 34(2): 48. CrossRef - Predisposition to and Prognosis of Thyroid Cancer May Not Be Affected by Graves’ Disease, But Some Questions Still Remain
Yanrui Huang, Haixia Guan
Clinical Thyroidology.2022; 34(2): 59. CrossRef - A Comparative Follow-Up Study of Patients with Papillary Thyroid Carcinoma Associated or Not with Graves’ Disease
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Maria Rondini, Angela Spanu, Giuseppe Madeddu
Diagnostics.2022; 12(11): 2801. CrossRef - An unusual case of papillary thyroid carcinoma presenting as Graves’ disease
Pooja Tiwari, Uma Kaimal Saikia, Abhamoni Baro, Ashok Krishna Bhuyan
Thyroid Research and Practice.2022; 19(1): 47. CrossRef
- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease

- Thyroid
- Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(5):1078-1085. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1151

- 3,883 View
- 110 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Hürthle cell carcinoma (HCC), a type of thyroid carcinoma, is rare in South Korea, and few studies have investigated its prognosis.
Methods
This long-term multicenter retrospective cohort study evaluated the clinicopathological features and clinical outcomes in patients with HCC who underwent thyroid surgery between 1996 and 2009.
Results
The mean age of the 97 patients included in the study was 50.3 years, and 26.8% were male. The mean size of the primary tumor was 3.2±1.8 cm, and three (3.1%) patients had distant metastasis at initial diagnosis. Ultrasonographic findings were available for 73 patients; the number of nodules with low-, intermediate-, and high suspicion was 28 (38.4%), 27 (37.0%), and 18 (24.7%), respectively, based on the Korean-Thyroid Imaging Reporting and Data System. Preoperatively, follicular neoplasm (FN) or suspicion for FN accounted for 65.2% of the cases according to the Bethesda category, and 13% had malignancy or suspicious for malignancy. During a median follow-up of 8.5 years, eight (8.2%) patients had persistent/recurrent disease, and none died of HCC. Older age, gross extrathyroidal extension (ETE), and widely invasive types of tumors were significantly associated with distant metastasis (all P<0.01). Gross ETE (hazard ratio [HR], 27.7; 95% confidence interval [CI], 2.2 to 346.4; P=0.01) and widely invasive classification (HR, 6.5; 95% CI, 1.1 to 39.4; P=0.04) were independent risk factors for poor disease-free survival (DFS).
Conclusion
The long-term prognosis of HCC is relatively favorable in South Korea from this study, although this is not a nation-wide data, and gross ETE and widely invasive cancer are significant prognostic factors for DFS. The diagnosis of HCC by ultrasonography and cytopathology remains challenging. -
Citations
Citations to this article as recorded by- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma
Lindsay A. Bischoff, Ian Ganly, Laura Fugazzola, Erin Buczek, William C. Faquin, Bryan R. Haugen, Bryan McIver, Caitlin P. McMullen, Kate Newbold, Daniel J. Rocke, Marika D. Russell, Mabel Ryder, Peter M. Sadow, Eric Sherman, Maisie Shindo, David C. Shonk
JAMA Otolaryngology–Head & Neck Surgery.2024; 150(3): 265. CrossRef - Oncocytic carcinoma of the thyroid: Conclusions from a 20‐year patient cohort
Nelson R. Gruszczynski, Shahzeb S. Hasan, Ana G. Brennan, Julian De La Chapa, Adithya S. Reddy, David N. Martin, Prem P. Batchala, Edward B. Stelow, Eric M. Dowling, Katherine L. Fedder, Jonathan C. Garneau, David C. Shonka
Head & Neck.2024;[Epub] CrossRef - Hurthle cell carcinoma: a rare variant of thyroid malignancy – a case report
Yuvraj Adhikari, Anupama Marasini, Nawaraj Adhikari, Laxman D. Paneru, Binit Upadhaya Regmi, Manita Raut
Annals of Medicine & Surgery.2023; 85(5): 1940. CrossRef - Hürthle Cell Carcinoma: Single Center Analysis and Considerations for Surgical Management Based on the Recent Literature
Costanza Chiapponi, Milan J.M. Hartmann, Matthias Schmidt, Michael Faust, Christiane J. Bruns, Anne M. Schultheis, Hakan Alakus
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma

- Thyroid
- Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
- Endocrinol Metab. 2021;36(4):717-724. Published online August 11, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1042
- Correction in: Endocrinol Metab 2022;37(1):180

- 4,694 View
- 180 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Active surveillance (AS) for low-risk papillary thyroid microcarcinoma (PTMC) has been accepted worldwide as safe and effective. Despite the growing acceptance of AS in the management of low-risk PTMCs, there are barriers to AS in real clinical settings, and it is important to understand and establish appropriate AS protocol from initial evaluation to follow-up. PTMC management strategies should be decided upon after careful consideration of patient and tumor characteristics by a multidisciplinary team of thyroid cancer specialists. Patients should understand the risks and benefits of AS, participate in decision-making and follow structured monitoring strategies. In this review, we discuss clinical outcomes of AS from previous studies, optimal indications and follow-up strategies for AS, and unresolved questions about AS.
-
Citations
Citations to this article as recorded by- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Papillary Thyroid Microcarcinoma: Active Surveillance Against Surgery. Considerations of an Italian Working Group From a Systematic Review
Giuseppina Orlando, Gregorio Scerrino, Alessandro Corigliano, Irene Vitale, Roberta Tutino, Stefano Radellini, Francesco Cupido, Giuseppa Graceffa, Gianfranco Cocorullo, Giuseppe Salamone, Giuseppina Melfa
Frontiers in Oncology.2022;[Epub] CrossRef - Prognosis of Patients with 1–4 cm Papillary Thyroid Cancer Who Underwent Lobectomy: Focus on Gross Extrathyroidal Extension Invading Only the Strap Muscles
Ahreum Jang, Meihua Jin, Won Woong Kim, Min Ji Jeon, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Yu-Mi Lee, Won Gu Kim
Annals of Surgical Oncology.2022; 29(12): 7835. CrossRef
- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma

- Clinical Study
- Gender-Dependent Reference Range of Serum Calcitonin Levels in Healthy Korean Adults
- Eyun Song, Min Ji Jeon, Hye Jin Yoo, Sung Jin Bae, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Hong-Kyu Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(2):365-373. Published online April 7, 2021
- DOI: https://doi.org/10.3803/EnM.2020.939

- 5,011 View
- 152 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Serum calcitonin measurement contains various clinical and methodological aspects. Its reference level is wide and unclear despite sensitive calcitonin kits are available. This study aimed to identify the specific reference range in the healthy Korean adults.
Methods
Subjects were ≥20 years with available calcitonin (measured by a two-site immunoradiometric assay) data by a routine health checkup. Three groups were defined as all eligible subjects (group 1, n=10,566); subjects without self or family history of thyroid disease (group 2, n=5,152); and subjects without chronic kidney disease, autoimmune thyroid disease, medication of proton pump inhibitor/H2 blocker/steroid, or other malignancies (group 3, n=4,638).
Results
This study included 6,341 male and 4,225 female subjects. Males had higher mean calcitonin than females (2.3 pg/mL vs. 1.9 pg/mL, P<0.001) in group 1. This gender difference remained similar in groups 2 and 3. Calcitonin according to age or body mass index was not significant in both genders. Higher calcitonin in smoking than nonsmoking men was observed but not in women. Sixty-nine subjects had calcitonin higher than the upper reference limit (10 pg/mL) and 64 of them had factors associated with hypercalcitoninemia besides medullary thyroid cancer. Our study suggests the reference intervals for men who were non, ex-, current smokers, and women (irrespective of smoking status) as <5.7, <7.1, <7.9, and <3.6 pg/mL, respectively.
Conclusion
Specific calcitonin reference range should be provided considering for sex and smoking status. Taking account for several factors known to induce hypercalcitoninemia can help interpret the gray zone of moderately elevated calcitonin. -
Citations
Citations to this article as recorded by- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma
Pierpaolo Trimboli, Giuseppe Peloni, Dorotea Confalonieri, Elena Gamarra, Tommaso Piticchio, Francesco Frasca, Petra Makovac, Arnoldo Piccardo, Lorenzo Ruinelli
Frontiers in Oncology.2024;[Epub] CrossRef - Surgical treatment of solid variant of papillary thyroid carcinoma: Fifteen-year experience of a tertiary center
Katarina Tausanović, Marina Stojanović, Milan Jovanović, Boban Stepanović, Jovan Ilić, Sara Ivaniš, Vladan Živaljević
Medicinska istrazivanja.2024; 57(1): 121. CrossRef - Some genetic differences in patients with rheumatoid arthritis
Hosam M. Ahmad, Zaki M. Zaki, Asmaa S. Mohamed, Amr E. Ahmed
BMC Research Notes.2023;[Epub] CrossRef - Presence or severity of Hashimoto’s thyroiditis does not influence basal calcitonin levels: observations from CROHT biobank
M. Cvek, A. Punda, M. Brekalo, M. Plosnić, A. Barić, D. Kaličanin, L. Brčić, M. Vuletić, I. Gunjača, V. Torlak Lovrić, V. Škrabić, V. Boraska Perica
Journal of Endocrinological Investigation.2022; 45(3): 597. CrossRef - Environmental Factors That Affect Parathyroid Hormone and Calcitonin Levels
Mirjana Babić Leko, Nikolina Pleić, Ivana Gunjača, Tatijana Zemunik
International Journal of Molecular Sciences.2021; 23(1): 44. CrossRef
- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma

- Clinical Study
- Clinical Outcomes after Early and Delayed Radioiodine Remnant Ablation in Patients with Low-Risk Papillary Thyroid Carcinoma: Propensity Score Matching Analysis
- Jonghwa Ahn, Meihua Jin, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Ji Min Han, Won Gu Kim
- Endocrinol Metab. 2020;35(4):830-837. Published online November 18, 2020
- DOI: https://doi.org/10.3803/EnM.2020.747
- 4,233 View
- 132 Download
- 3 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
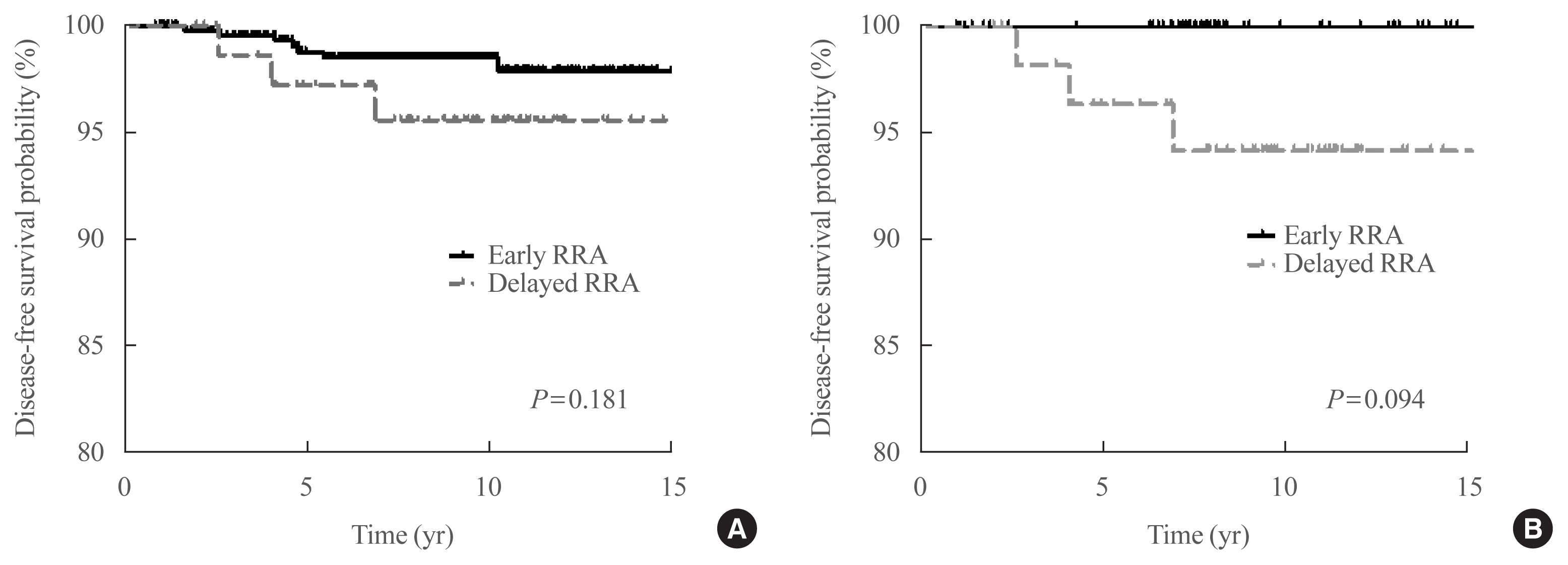
The clinical outcomes of delayed radioiodine remnant ablation (RRA) therapy in patients with low-risk papillary thyroid carcinoma (PTC) are unclear. We aimed to evaluate the clinical impact of the interval between total thyroidectomy (TT) and RRA therapy in patients with low-risk PTC.
Methods
We included 526 patients who underwent TT and RRA for low-risk PTC with a primary tumor size of >1 cm between 2000 and 2012. Patients were divided into the early (<90 days) and the delayed (≥90 days) RRA groups based on the interval between TT and RRA. The results of diagnostic whole-body scan (DxWBS), ongoing risk stratification (ORS; response to therapy), and disease-free survival (DFS) were evaluated before and after propensity score matching (PSM).
Results
Among the 526 patients, 75 (14.3%) patients underwent delayed RRA; they had more cervical lymph node metastasis and received a higher RRA dose than those who underwent early RRA. The median follow-up period was 9.1 years after initial therapy, and the structural recurrence rate was 1.9%. In DxWBS, 60 patients had focal iodine uptake limited in operative bed, with no significant difference between groups. According to ORS, 78%, 20%, 1%, and 1% patients were classified into excellent, indeterminate, biochemical incomplete, and structural incomplete response groups, respectively. There was no significant difference in ORS or DFS between groups before and after PSM.
Conclusion
The timing of the first RRA had no clinical impact in patients with low-risk PTC. Thus, the clinical decision for RRA can be determined >3 months after TT considering other prognostic factors. -
Citations
Citations to this article as recorded by- Dynamic risk assessment in patients with differentiated thyroid cancer
Erika Abelleira, Fernando Jerkovich
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 79. CrossRef - Ablation Rates and Long-Term Outcome Following Low-Dose Radioiodine for Differentiated Thyroid Cancer in the West of Scotland: A Retrospective Analysis
Kathryn Graham, Fay Tough, Helena Belikova, Irene Wotherspoon, David Colville, Nicholas Reed
Endocrine Practice.2024; 30(4): 327. CrossRef - Radioiodine ablation after thyroidectomy could be safely abandoned or postponed in selected stage I papillary thyroid carcinoma patients of low-risk group: an observational prospective study
S.M. Cherenko, A.Yu. Glagolieva, D.E. Makhmudov
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2024; 20(1): 7. CrossRef - Patient Preparation and Radiation Protection Guidance for Adult Patients Undergoing Radioiodine Treatment for Thyroid Cancer in the UK
J. Wadsley, N. Armstrong, V. Bassett-Smith, M. Beasley, R. Chandler, L. Cluny, A.J. Craig, K. Farnell, K. Garcez, N. Garnham, K. Graham, A. Hallam, S. Hill, H. Hobrough, F. McKiddie, M.W.J. Strachan
Clinical Oncology.2023; 35(1): 42. CrossRef - Delay of initial radioactive iodine therapy beyond 3 months has no effect on clinical responses and overall survival in patients with thyroid carcinoma: A cohort study and a meta‐analysis
Fang Cheng, Juan Xiao, Fengyan Huang, Chunchun Shao, Shouluan Ding, Canhua Yun, Hongying Jia
Cancer Medicine.2022; 11(12): 2386. CrossRef - Delayed (>3 Months) Postoperative Radioactive Iodine Ablation Does Not Impact Clinical Response or Survival in Differentiated Thyroid Cancers
Tatiana Fedorova, Lilah F. Morris-Wiseman
Clinical Thyroidology.2022; 34(10): 456. CrossRef
- Dynamic risk assessment in patients with differentiated thyroid cancer

- Clinical Study
- Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2020;35(3):618-627. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.742
- 5,401 View
- 121 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
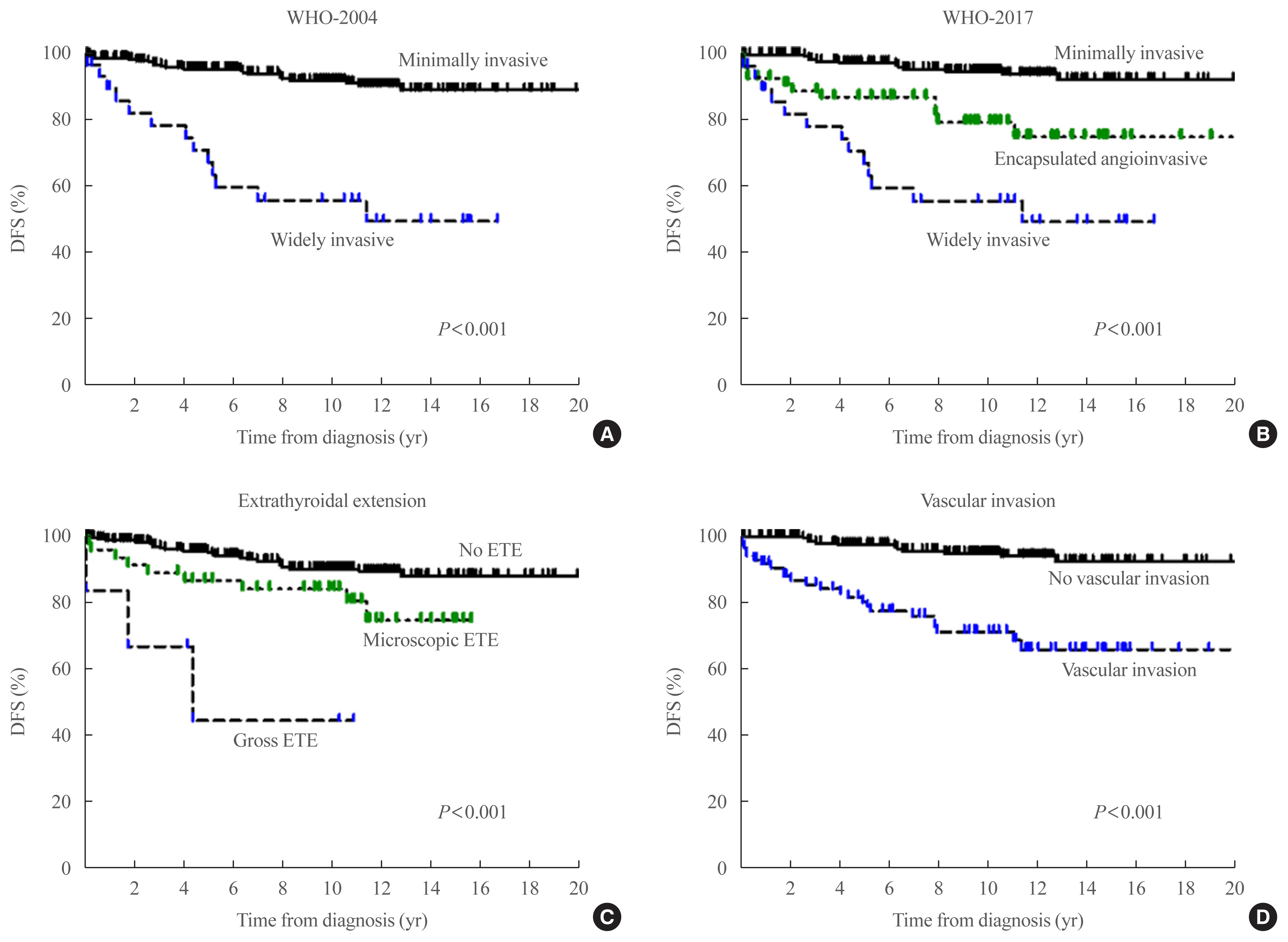
The study aimed to compare the prognostic value of the 4th edition of World Health Organization classification (WHO-2017) with the previous WHO classification (WHO-2004) for follicular thyroid carcinoma (FTC).
Methods
This multicenter retrospective cohort study included 318 patients with FTC from five tertiary centers who underwent thyroid surgery between 1996 and 2009. We evaluated the prognosis of patients with minimally invasive (MI), encapsulated angioinvasive (EA), and widely invasive (WI) FTC according to WHO-2017. Further, we evaluated the proportion of variation explained (PVE) and Harrell’s C-index to compare the predictability of disease-free survival (DFS) and disease-specific survival (DSS).
Results
In total, 227, 58, and 33 patients had MI-, EA-, and WI-FTC, respectively. During a median follow-up of 10.6 years, 46 (14.5%) patients had disease recurrence and 20 (6.3%) patients died from FTC. The 10-year DFS rates of patients with MI-, EA-, and WI-FTC were 91.1%, 78.2%, and 54.9%, respectively (P<0.001, PVE=7.1%, C-index=0.649). The corresponding 10-year DSS rates were 95.9%, 93.5%, and 73.5%, respectively (P<0.001, PVE=2.6%, C-index=0.624). The PVE and C-index values were higher using WHO-2017 than using WHO-2004 for the prediction of DFS, but not for DSS. In multivariate analysis, older age (P=0.02), gross extrathyroidal extension (ETE) (P=0.003), and distant metastasis (P<0.001) were independent risk factors for DSS.
Conclusion
WHO-2017 improves the predictability of DFS, but not DSS, in patients with FTC. Distant metastasis, gross ETE and older age (≥55 years) were independent risk factors for DSS. -
Citations
Citations to this article as recorded by- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation
Myoung Kyoung Kim, Hyunju Park, Young Lyun Oh, Jung Hee Shin, Tae Hyuk Kim, Soo Yeon Hahn
Korean Journal of Radiology.2024; 25(1): 103. CrossRef - Clinical Outcomes and Implications of Radioactive Iodine Therapy on Cancer-specific Survival in WHO Classification of FTC
Genpeng Li, Ziyang Ye, Tao Wei, Jingqiang Zhu, Zhihui Li, Jianyong Lei
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Radioiodine whole body scan pitfalls in differentiated thyroid cancer
Cristina Basso, Alessandra Colapinto, Valentina Vicennati, Alessandra Gambineri, Carla Pelusi, Guido Di Dalmazi, Elisa Lodi Rizzini, Elena Tabacchi, Arber Golemi, Letizia Calderoni, Stefano Fanti, Uberto Pagotto, Andrea Repaci
Endocrine.2024;[Epub] CrossRef - The Prognostic Impact of Extent of Vascular Invasion in Follicular Thyroid Carcinoma
David Leong, Anthony J. Gill, John Turchini, Michael Waller, Roderick Clifton‐Bligh, Anthony Glover, Mark Sywak, Stan Sidhu
World Journal of Surgery.2023; 47(2): 412. CrossRef - TERT Promoter Mutation as a Prognostic Marker in Encapsulated Angioinvasive and Widely Invasive Follicular Thyroid Carcinomas
Yasuhiro Ito, Takashi Akamizu
Clinical Thyroidology.2023; 35(5): 202. CrossRef - Risk factors for death of follicular thyroid carcinoma: a systematic review and meta-analysis
Ting Zhang, Liang He, Zhihong Wang, Wenwu Dong, Wei Sun, Ping Zhang, Hao Zhang
Endocrine.2023; 82(3): 457. CrossRef - Molecular classification of follicular thyroid carcinoma based on TERT promoter mutations
Hyunju Park, Hyeong Chan Shin, Heera Yang, Jung Heo, Chang-Seok Ki, Hye Seung Kim, Jung-Han Kim, Soo Yeon Hahn, Yun Jae Chung, Sun Wook Kim, Jae Hoon Chung, Young Lyun Oh, Tae Hyuk Kim
Modern Pathology.2022; 35(2): 186. CrossRef - Whole-genome Sequencing of Follicular Thyroid Carcinomas Reveal Recurrent Mutations in MicroRNA Processing Subunit DGCR8
Johan O Paulsson, Nima Rafati, Sebastian DiLorenzo, Yi Chen, Felix Haglund, Jan Zedenius, C Christofer Juhlin
The Journal of Clinical Endocrinology & Metabolism.2021; 106(11): 3265. CrossRef - Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2021; 36(5): 1078. CrossRef
- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation

- Clinical Study
- Clinical Outcomes of N1b Papillary Thyroid Cancer Patients Treated with Two Different Doses of Radioiodine Ablation Therapy
- Meihua Jin, Jonghwa Ahn, Yu-Mi Lee, Tae-Yon Sung, Won Gu Kim, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon
- Endocrinol Metab. 2020;35(3):602-609. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.741

- 5,397 View
- 121 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The optimal dose of radioactive iodine (RAI) therapy for N1b papillary thyroid carcinoma (PTC) is controversial. We evaluated the clinical outcome of N1b PTC patients treated with either 100 or 150 mCi of RAI.
Methods
We retrospectively analyzed N1b PTC patients who underwent total thyroidectomy and postoperative RAI therapy at a tertiary referral center between 2012 and 2017. As the baseline characteristics differed between treatment groups, we performed exact matching for various pathological factors according to RAI dose. We evaluated the response to therapy and recurrence-free survival (RFS) in the matched patients. Structural recurrent/persistent disease was defined as new structural disease detected after initial therapy, which was confirmed by cytology or pathology.
Results
Of the total 436 patients, 37 (8.5%) received 100 mCi of RAI and 399 (91.5%) received 150 mCi of RAI. After an exact 1:3 matching, 34 patients in the 100 mCi group and 100 patients in the 150 mCi group remained. There was no significant difference in response to therapy between the groups in the matched population (P=0.63). An excellent response was achieved in 70.6% (n=24) of patients in the 100 mCi group and 76.0% (n=76) in the 150 mCi group. Two (5.9%) patients in the 100 mCi group and four (4.0%) in the 150 mCi group had recurrence and there was no significant difference in RFS between the groups in the matched population (P=0.351).
Conclusion
There were no differences in response to therapy and RFS in N1b PTC patients according to RAI dose.

- Clinical Study
- Vandetanib for the Management of Advanced Medullary Thyroid Cancer: A Real-World Multicenter Experience
- Mijin Kim, Jee Hee Yoon, Jonghwa Ahn, Min Ji Jeon, Hee Kyung Kim, Dong Jun Lim, Ho-Cheol Kang, In Joo Kim, Young Kee Shong, Tae Yong Kim, Bo Hyun Kim
- Endocrinol Metab. 2020;35(3):587-594. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.687

- 5,628 View
- 146 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Vandetanib is the most widely used tyrosine kinase inhibitor for the treatment of patients with advanced medullary thyroid cancer (MTC). However, only limited data regarding its use outside clinical trials are available. We aimed to evaluate the efficacy and safety of vandetanib in patients with advanced MTC in routine clinical practice.
Methods
In this multicenter retrospective study, 12 patients with locally advanced or metastatic MTC treated with vandetanib at four tertiary hospitals were included. The primary outcome was the objective response rate (ORR) based on the Response Evaluation Criteria in Solid Tumors. The progression-free survival (PFS), overall survival (OS), and toxicities were also evaluated.
Results
Eleven patients (92%) had distant metastasis and 10 (83%) had disease progression at enrollment. Partial response was observed in five patients (ORR, 42%) and stable disease lasting ≥24 weeks was reported in an additional five patients (83%). During the median 31.7 months of follow-up, disease progression was seen in five patients (42%); of these, two died due to disease progression. The median PFS was 25.9 months, while the median OS was not reached. All patients experienced adverse events (AEs) which were generally consistent with the known safety profile of vandetanib. Vandetanib was discontinued in two patients due to skin toxicity.
Conclusion
Consistent with the phase III trial, this study confirmed the efficacy of vandetanib for advanced MTC in terms of both ORR and PFS in the real-world setting. Vandetanib was well tolerated in the majority of patients, and there were no fatal AEs. -
Citations
Citations to this article as recorded by- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance
Katerina Saltiki, George Simeakis, Olga Karapanou, Stavroula A. Paschou, Maria Alevizaki
Endocrine.2023; 80(3): 570. CrossRef - Initial Experiences of Selective RET Inhibitor Selpercatinib in Adults with Metastatic Differentiated Thyroid Carcinoma and Medullary Thyroid Carcinoma: Real-World Case Series in Korea
Han-Sang Baek, Jeonghoon Ha, Seunggyun Ha, Ja Seong Bae, Chan Kwon Jung, Dong-Jun Lim
Current Oncology.2023; 30(3): 3020. CrossRef - Molecular Basis and Natural History of Medullary Thyroid Cancer: It is (Almost) All in the RET
Nicolas Sahakian, Frédéric Castinetti, Pauline Romanet
Cancers.2023; 15(19): 4865. CrossRef - Sporadic Medullary Thyroid Carcinoma: Towards a Precision Medicine
Antonio Matrone, Carla Gambale, Alessandro Prete, Rossella Elisei
Frontiers in Endocrinology.2022;[Epub] CrossRef - Targeted therapy and drug resistance in thyroid cancer
Yujie Zhang, Zhichao Xing, Tianyou Liu, Minghai Tang, Li Mi, Jingqiang Zhu, Wenshuang Wu, Tao Wei
European Journal of Medicinal Chemistry.2022; 238: 114500. CrossRef - Daily Management of Patients on Multikinase Inhibitors’ Treatment
Carla Colombo, Simone De Leo, Matteo Trevisan, Noemi Giancola, Anna Scaltrito, Laura Fugazzola
Frontiers in Oncology.2022;[Epub] CrossRef - The Angiogenic Balance and Its Implications in Cancer and Cardiovascular Diseases: An Overview
Cătălina Ionescu, Bogdan Oprea, Georgeta Ciobanu, Milena Georgescu, Ramona Bică, Garofiţa-Olivia Mateescu, Fidan Huseynova, Veronique Barragan-Montero
Medicina.2022; 58(7): 903. CrossRef - Reassessing vascular endothelial growth factor (VEGF) in anti-angiogenic cancer therapy
Tobiloba C. Elebiyo, Damilare Rotimi, Ikponmwosa O. Evbuomwan, Rotdelmwa Filibus Maimako, Matthew Iyobhebhe, Oluwafemi Adeleke Ojo, Olarewaju M. Oluba, Oluyomi S. Adeyemi
Cancer Treatment and Research Communications.2022; 32: 100620. CrossRef - Current Guidelines for Management of Medullary Thyroid Carcinoma
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(3): 514. CrossRef - Recent advances in precision medicine for the treatment of medullary thyroid cancer
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Barbara Jarzab
Expert Review of Precision Medicine and Drug Development.2021; 6(5): 307. CrossRef - Functional evaluation of vandetanib metabolism by CYP3A4 variants and potential drug interactions in vitro
Mingming Han, Xiaodan Zhang, Zhize Ye, Jing Wang, Jianchang Qian, Guoxin Hu, Jianping Cai
Chemico-Biological Interactions.2021; 350: 109700. CrossRef - Nephrotoxicity in advanced thyroid cancer treated with tyrosine kinase inhibitors: An update
Alice Nervo, Francesca Retta, Alberto Ragni, Alessandro Piovesan, Alberto Mella, Luigi Biancone, Marco Manganaro, Marco Gallo, Emanuela Arvat
Critical Reviews in Oncology/Hematology.2021; 168: 103533. CrossRef
- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance

- Clinical Study
- Modification of the Tumor-Node-Metastasis Staging System for Differentiated Thyroid Carcinoma by Considering Extra-Thyroidal Extension and Lateral Cervical Lymph Node Metastasis
- Mijin Kim, Won Gu Kim, Min Ji Jeon, Hee Kyung Kim, Hyon-Seung Yi, Eun Sook Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Ho-Cheol Kang, Tae Yong Kim
- Endocrinol Metab. 2020;35(1):149-156. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.149
- 5,244 View
- 82 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
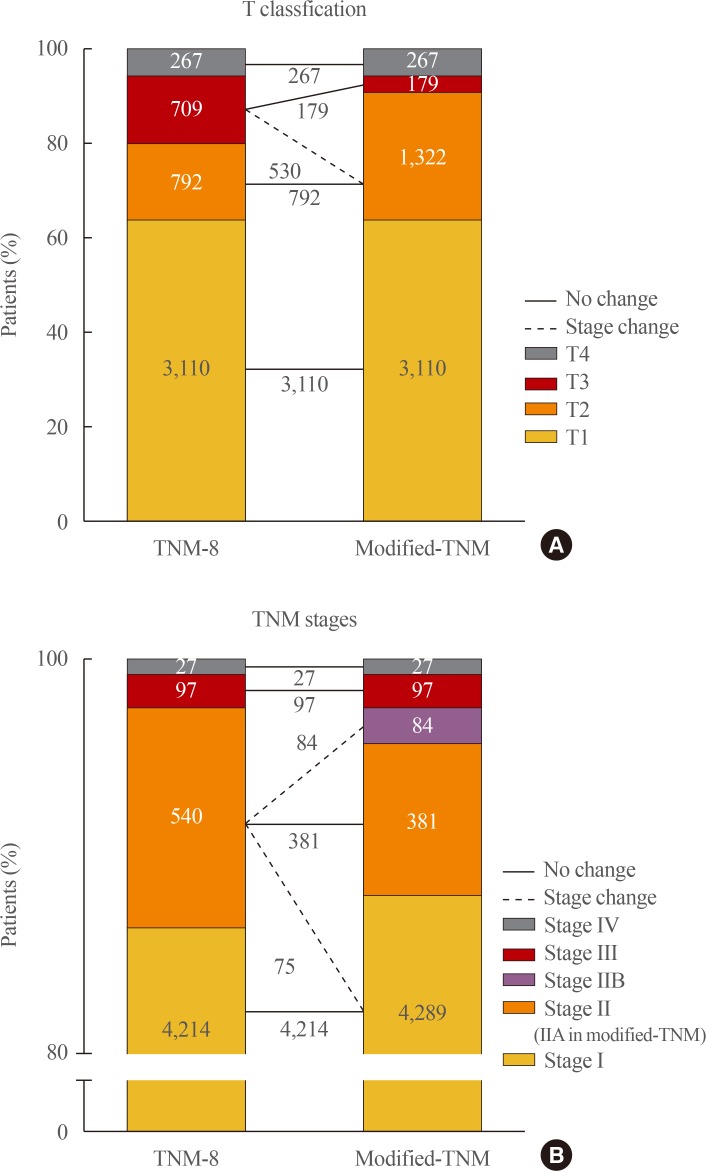
ePub Background Concerns have arisen about the classification of extra-thyroidal extension (ETE) and lateral cervical lymph node metastasis (N1b) in the 8th edition of the tumor-node-metastasis staging system (TNM-8). This study evaluated the prognostic validity of a modified-TNM staging system, focusing on ETE and N1b, in differentiated thyroid carcinoma (DTC) patients.
Methods This multicenter retrospective cohort study included 4,878 DTC patients from five tertiary hospitals. In the modified-TNM, T3b in TNM-8 was down-staged to T2, and stage II was subdivided into stages IIA and IIB. Older patients with N1b were reclassified as stage IIB.
Results The modified-TNM resulted in staging migration in 540 patients (11%) classified as stage II according to the TNM-8, with 75 (14%), 381 (71%), and 84 patients (16%) classified as stages I, IIA, and IIB, respectively. The 10-year disease-specific survival (DSS) rates in patients classified as stages I, II, III, and IV by TNM-8 were 99.8%, 95.9%, 81.0%, and 41.6%, respectively. The DSS rates of patients classified as stages I, IIA, IIB, III, and IV according to the modified-TNM were 99.8%, 96.4%, 93.3%, 81.0%, and 41.6%, respectively. DSS curves between stages on TNM-8 (
P <0.001) and modified-TNM (P <0.001) differed significantly, but the modified-TNM discriminated better than TNM-8. The proportions of variation explained values of TNM-8 and modified-TNM were 6.3% and 6.5%, respectively.Conclusion Modification of the TNM staging system focusing on ETE and N1b could improve the prediction of DSS in patients with DTC. Further researches are needed to validate the prognostic accuracy of this modified-TNM staging system.
-
Citations
Citations to this article as recorded by- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy
Wen Liu, Beibei Jiang, Jingli Xue, Ruijing Liu, Yuqing Wei, Peifeng Li
Annals of Diagnostic Pathology.2024; 69: 152243. CrossRef - Thyroid Collision Tumors: The Presence of the Medullary Thyroid Carcinoma Component Negatively Influences the Prognosis
Ion Negura, Victor Ianole, Mihai Danciu, Cristina Preda, Diana Gabriela Iosep, Radu Dănilă, Alexandru Grigorovici, Delia Gabriela Ciobanu Apostol
Diagnostics.2023; 13(2): 285. CrossRef - Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Prognostic Impact of Microscopic Extra-Thyroidal Extension (mETE) on Disease Free Survival in Patients with Papillary Thyroid Carcinoma (PTC)
Nadia Bouzehouane, Pascal Roy, Myriam Decaussin-Petrucci, Mireille Bertholon-Grégoire, Chantal Bully, Agnès Perrin, Helene Lasolle, Jean-Christophe Lifante, Françoise Borson-Chazot, Claire Bournaud
Cancers.2022; 14(11): 2591. CrossRef - Impacts of the American Joint Committee on Cancer (AJCC) 8th edition tumor, node, metastasis (TNM) staging system on outcomes of differentiated thyroid cancer in Thai patients
Yotsapon Thewjitcharoen, Waralee Chatchomchuan, Krittadhee Karndumri, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Veekij Veerasomboonsin, Auchai Kanchanapituk, Rajata Rajatanavin, Thep Himatho
Heliyon.2021; 7(3): e06624. CrossRef
- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy

- Thyroid
- Unmet Clinical Needs in the Treatment of Patients with Thyroid Cancer
- Won Bae Kim, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong
- Endocrinol Metab. 2020;35(1):14-25. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.14
- 7,061 View
- 135 Download
- 14 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
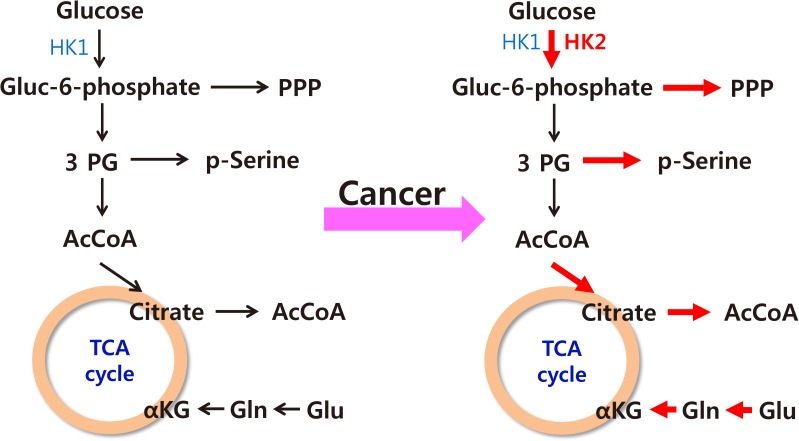
ePub The increased incidence of thyroid cancer is a worldwide phenomenon; however, the issue of overdiagnosis has been most prominent in South Korea. The age-standardized mortality rate of thyroid cancer in Korea steeply increased from 1985 to 2004 (from 0.17 per 100,000 to 0.85 per 100,000), and then decreased until 2015 to 0.42 per 100,000, suggesting that early detection reduced mortality. However, early detection of thyroid cancer may be cost-ineffective, considering its very high prevalence and indolent course. Therefore, risk stratification and tailored management are vitally important, but many prognostic markers can only be evaluated postoperatively. Discovery of preoperative marker(s), especially for small cancers, is the most important unmet clinical need for thyroid cancer. Herein, we discuss some such factors that we recently discovered. Another unmet clinical need is better treatment of radioiodine-refractory (RAIR) differentiated thyroid cancer (DTC) and undifferentiated cancers. Although sorafenib and lenvatinib are available, better drugs are needed. We found that phosphoglycerate dehydrogenase, a critical enzyme for serine biosynthesis, could be a novel therapeutic target, and that the lymphocyte-to-monocyte ratio is a prognostic marker of survival in patients with anaplastic thyroid carcinoma or RAIR DTC. Deeper insights are needed into tumor-host interactions in thyroid cancer to improve treatment.
-
Citations
Citations to this article as recorded by- Lenvatinib Compared with Sorafenib as a First-Line Treatment for Radioactive Iodine-Refractory, Progressive, Differentiated Thyroid Carcinoma: Real-World Outcomes in a Multicenter Retrospective Cohort Study
Mijin Kim, Meihua Jin, Min Ji Jeon, Eui Young Kim, Dong Yeob Shin, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Hee Kyung Kim, Won Gu Kim
Thyroid.2023; 33(1): 91. CrossRef - Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Integration of ultrasound-based radiomics with clinical features for predicting cervical lymph node metastasis in postoperative patients with differentiated thyroid carcinoma
Fengjing Fan, Fei Li, Yixuan Wang, Zhengjun Dai, Yuyang Lin, Lin Liao, Bei Wang, Hongjun Sun
Endocrine.2023;[Epub] CrossRef - Transcriptomic Analysis of Papillary Thyroid Cancer: A Focus on Immune-Subtyping, Oncogenic Fusion, and Recurrence
Seung-Jin Park, Yea Eun Kang, Jeong-Hwan Kim, Jong-Lyul Park, Seon-Kyu Kim, Seung-Woo Baek, In Sun Chu, Shinae Yi, Seong Eun Lee, Young Joo Park, Eun-Jae Chung, Jin Man Kim, Hye Mi Ko, Je-Ryong Kim, Seung-Nam Jung, Ho-Ryun Won, Jae Won Chang, Bon Seok Koo
Clinical and Experimental Otorhinolaryngology.2022; 15(2): 183. CrossRef - Prognosis of Patients with 1–4 cm Papillary Thyroid Cancer Who Underwent Lobectomy: Focus on Gross Extrathyroidal Extension Invading Only the Strap Muscles
Ahreum Jang, Meihua Jin, Won Woong Kim, Min Ji Jeon, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Yu-Mi Lee, Won Gu Kim
Annals of Surgical Oncology.2022; 29(12): 7835. CrossRef - Carboxy terminus of HSP70‐interacting protein (CHIP) attenuates the stemness of thyroid cancer cells through decreasing OCT4 protein stability
Ying Xu, Gang Xu, Huimin Dang, Wei Qu, Dan Chang, Xin He, Minmin Li, Qian Wang
Environmental Toxicology.2021; 36(4): 686. CrossRef - Lactate Dehydrogenase A as a Potential New Biomarker for Thyroid Cancer
Eun Jeong Ban, Daham Kim, Jin Kyong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Kunhong Kim
Endocrinology and Metabolism.2021; 36(1): 96. CrossRef - Clinical implications of age and excellent response to therapy in patients with high‐risk differentiated thyroid carcinoma
Meihua Jin, Jonghwa Ahn, Yu‐Mi Lee, Tae‐Yon Sung, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Won Gu Kim
Clinical Endocrinology.2021; 95(6): 882. CrossRef - CD73 Overexpression Promotes Progression and Recurrence of Papillary Thyroid Carcinoma
Young Mun Jeong, Haejin Cho, Tae-Min Kim, Yourha Kim, Sora Jeon, Andrey Bychkov, Chan Kwon Jung
Cancers.2020; 12(10): 3042. CrossRef - The Role of Exosomes in Thyroid Cancer and Their Potential Clinical Application
Kaixiang Feng, Runsheng Ma, Lele Zhang, Hongqiang Li, Yifeng Tang, Gongbo Du, Dongpeng Niu, Detao Yin
Frontiers in Oncology.2020;[Epub] CrossRef
- Lenvatinib Compared with Sorafenib as a First-Line Treatment for Radioactive Iodine-Refractory, Progressive, Differentiated Thyroid Carcinoma: Real-World Outcomes in a Multicenter Retrospective Cohort Study

- Clinical Study
- Quality of Life in Patients with Papillary Thyroid Microcarcinoma According to Treatment: Total Thyroidectomy with or without Radioactive Iodine Ablation
- Jonghwa Ahn, Min Ji Jeon, Eyun Song, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
- Endocrinol Metab. 2020;35(1):115-121. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.115
- 5,484 View
- 110 Download
- 8 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
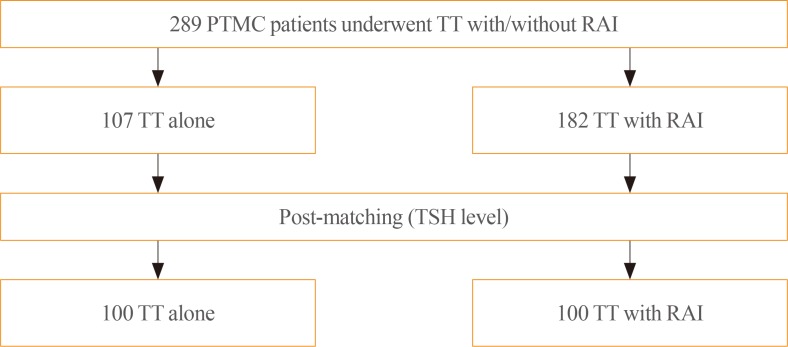
ePub Background Recently, there has been some controversy regarding the role of radioactive iodine (RAI) ablation in the treatment of low-risk differentiated thyroid carcinoma (DTC), especially papillary thyroid microcarcinoma (PTMC). This study aimed to compare quality of life (QoL) parameters between patients with PTMC who underwent total thyroidectomy (TT) alone and those who underwent TT with RAI ablation.
Methods In this cross-sectional study, patients with PTMC who underwent TT with/without RAI remnant ablation were prospectively enrolled between June 2016 and October 2017. All patients completed three questionnaires: the 12-item short-form health survey (SF-12), thyroid cancer-specific quality of life (THYCA-QoL) questionnaire, and fear of progression (FoP) questionnaire.
Results The TT and TT with RAI groups comprised 107 and 182 patients, respectively. The TT with RAI group had significantly lower serum thyrotropin (TSH) levels than the TT group. However, after matching for TSH levels between the groups (
n =100 in both groups), there were no significant differences in baseline characteristics. According to the SF-12, the score for general health was significantly lower in the TT with RAI group than in the TT group (P =0.047). The THYCA-QoL also showed a significant difference in the “felt chilly” score between groups (P =0.023). No significant differences in FoP scores were observed between the groups.Conclusion Patients with PTMC who underwent TT with RAI ablation experienced more health-related problems than those managed with TT alone. These findings support the idea that RAI ablation should be carefully considered in patients with low-risk DTCs.
-
Citations
Citations to this article as recorded by- Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición.2024; 71(2): 61. CrossRef - Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición (English ed.).2024; 71(2): 61. CrossRef - Fear of Cancer Recurrence in Differentiated Thyroid Cancer Survivors: A Systematic Review
Jacob Hampton, Ahmad Alam, Nicholas Zdenkowski, Christopher Rowe, Elizabeth Fradgley, Christine J. O'Neill
Thyroid®.2024;[Epub] CrossRef - Review: Improving quality of life in patients with differentiated thyroid cancer
Pia Pace-Asciak, Jonathon O. Russell, Ralph P. Tufano
Frontiers in Oncology.2023;[Epub] CrossRef - Health-Related Quality of Life and Thyroid Cancer-Specific Symptoms in Patients Treated for Differentiated Thyroid Cancer: A Single-Center Cross-Sectional Survey from Mainland China
Changlian Chen, Jiayan Cao, Yueyang Wang, Xuya Han, Yaju Zhang, Shumei Zhuang
Thyroid.2023; 33(4): 474. CrossRef - The "not so good" thyroid cancer: a scoping review on risk factors associated with anxiety, depression and quality of life
Kyle Alexander, Sum-Yu Christina Lee, Stelios Georgiades, Constantina Constantinou
Journal of Medicine and Life.2023; 16(3): 348. CrossRef - Comparison of health‐related quality of life and cosmetic outcome between traditional gasless trans‐axillary endoscopic thyroidectomy and modified gasless trans‐axillary endoscopic thyroidectomy for patients with papillary thyroid microcarcinoma
Deenraj Kush Dhoomun, HuiLan Cai, Ning Li, YanHuan Qiu, XingRui Li, XiaoPeng Hu, WenZhuang Shen
Cancer Medicine.2023; 12(15): 16604. CrossRef - Risk of Adverse Pregnancy Outcomes in Young Women with Thyroid Cancer: A Systematic Review and Meta-Analysis
Shinje Moon, Ka Hee Yi, Young Joo Park
Cancers.2022; 14(10): 2382. CrossRef - Health-related quality of life following FDG-PET/CT for cytological indeterminate thyroid nodules
Elizabeth J de Koster, Olga Husson, Eveline W C M van Dam, G Sophie Mijnhout, Romana T Netea-Maier, Wim J G Oyen, Marieke Snel, Lioe-Fee de Geus-Oei, Dennis Vriens, _ _
Endocrine Connections.2022;[Epub] CrossRef - Is a four-week hormone suspension necessary for thyroid remnant ablation in low and intermediate risk patients? A pilot study with quality-of-life assessment
Poliane A.L. Santos, Maria E.D.M. Flamini, Felipe A. Mourato, Fernando R.A. Lima, Joelan A.L. Santos, Fabiana F. Lima, Estelita T.B. Albuquerque, Alexandra C. De Freitas, Simone C.S. Brandão
Brazilian Journal of Radiation Sciences.2022; 10(4): 1. CrossRef - Health-related quality of life after transoral robotic thyroidectomy in papillary thyroid carcinoma
Chang Myeon Song, Hyang Sook Bang, Hyung Gu Kim, Hae Jin Park, Kyung Tae
Surgery.2021; 170(1): 99. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef
- Quality of life of patients with thyroid cancer in Colombia

- Clinical Features of Multiple Endocrine Neoplasia Type I in Koreans.
- Chul Hee Kim, Ghi Su Kim, Hong Kyu Kim, Joong Yeol Park, Young Kee Shong, Ki Up Lee
- J Korean Endocr Soc. 1996;11(2):163-174. Published online November 7, 2019
- 1,146 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Multiple endocrine neoplasia type I(MEN I) is a rare, eomplex, and potentially lethal disease. In Korean, only five anecdotal cases were reported as yet. The authors rescently experienced four cases of MEN I, and analysed the clinieal characteristics of MEN I in Koreans. Methods: The authors evaluated nine cases of MEN I, retrospectively. Four cases were analysed by clinical records in patients admitted to Asan Medical Center and five cases were reviewed by previously reported Korean literature from 1986 to 1995. Results: The average age was 39 years(ranged from 33 to 59 years). Eight of the nine patients had hyperparathyroidism documented by elevated serum calcium and PTH level with or without evidence of parathyroid mass. Initial presenting manifestations were symptomatic urinary stone, hypoglycernia due to insulinoma, hypogonadism, acromegaly, or peptic ulcer. Eight of nine patients had pancreatic islet cell tumors, and three of them were be malignant by radiologic and/or pathologic findings. The pancreatic tumors produced various hormones, such as gastrin, insulin, glucagon, or combination of them. Six of the nine cases had pituitary lesion. The most cornmon pituitary tumor was prolactinoma and the remaining was GH or GH and TSH producing tumor. In addition to the major components of MEN I, four had adrenocortical hyperplasia or adenoma and two had carcinoid tumor. There was only one familial case. Conclusion: The clinical charateristics of MEN I in Korean are mostly not different from the previous reports except older age at diagnosis, more comrnon adrenal involvement(44%) and gastrointestinal carcinoid tumor(22%). Although only one case was familial, more cases could be found if careful screening were done for the family members of the MBN I patients. In addition, screening and close follow up for endocrine pancreatic tumors are required for MEN I patients without detectable pancreatic lesion becau~se the malignant potential of pancreatic tumors has beeome an increasing concem for the prognosis of MEN I.

- Autoantigenic Role of Variant Thyroperoxidase.
- Young Kee Shong, Dae Hyuk Moon, Ghi Su Kim
- J Korean Endocr Soc. 1996;11(1):61-67. Published online November 7, 2019
- 1,054 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Thyroperoxidase(TPO) is one of the most important autoantigens in autoimmune thyroid disorders and autoantibody to TPO is found in almost every patients with various autoimmune thyroid diseases. Human TPO was already cloned and the completed nucleotide sequences are well known. In human thyroid tissues, several variants mRNA's of TPO are found in addition to the wild type. Especially the variants lacking exon 10(TPOΔexon10) and exon 16(TPOΔ exon16) are found in very large amount in both normal and Graves thyroid tissues. The significance of these variants TPO mRNAs are largely unknown. The authors tried to investigate the autoantigenic role of these variant TPO. Methods : To produce variant TPO cDNAs, oligonucleotide directed mutagenesis was performed using cDNA for wild type human TPO as template. The produced variants cDNAs were transfected into Cos-7 cells and variants TPO proteins were tested against patients sera showing high titers of anti-TPO antibody. Results: Seven of 12 Graves sera reacted with TPOΔexon 10 and 8 Graves sera with TPOΔ exonl6. Eight of 15 Hashimoto sera reacted TPOΔexon16 and 9 with TPOΔexon16. The reactivity with variants TPO was not related to clinical findings. Conclusion: These two variant TPOs, that is TPOexon10 and TPOΔexon16, could act as an autoantigen if they were translated in vivo, and could play a role in autoimmune thyroid disease. Their exact role in the pathogenesis of autoimmune thyroid disorders are to be clarified.

- Difference of Thyroid Stimulating Antidody Activities Measured in Chinese Hamster Ovary Cells Stably Transfected with Human TSH Receptor and in FRTL-5 Cells in Graves Disease and Its Clinical Correlations.
- Young Kee Shong Young Kee Shong, Hye Young Park, Bo Youn Cho, Won Bae Kim, Hong Gyu Lee, Chang Soon Koh, Yeon Sang Oh
- J Korean Endocr Soc. 1996;11(1):18-29. Published online November 7, 2019
- 1,110 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Background
: Thyroid stimulating antibodies result in the development of hyperthyroidism and goiter in Graves disease. However, thyroid stimulating antibody activities do not correlate with the clinical features in many patients with Graves disease. The purpose of this study is to address this discrepancy between thyroid stimulating antibody activities and clinical features of Graves patients. Methods: We measured thyroid stimulating antibody activities simultaneously using human TSH receptor transfected Chinese hamster(hTSHR-CHO) cells and rat thyroid(FRTL-5) cells in 57 untreated patients with Graves disease, and compared their activities with clinical features including thyroid hormone levels. Results : The detection rate of thyroid stimulating antibody measured by hTSHR-CHO cells was 90% in 57 untreated Graves patients and it was higher than that measured by FRTL-5 cells. Thyroid stimulating antibody activity by hTSHR-CHO cells was significantly correlated with that by FRTL-5 cells(r=0.5, p<0.001), however, 18 of 57(32%) patients showed marked discrepancy of thyroid stimulating antibody activity between in hTSHR-CHO and FRTL-5 systems. Thyroid stimulating antibody activity measured by hTSHR-CHO cells was significantly correlated with serum total T3, free T4 levels, and goiter size but not 99mTc-thyroid uptake. On the other hand, thyroid stimulating antibody activity measured by FRTL-5 cells was significantly correlated with goiter size and 99mTc-thyroid uptake but not thyroid hormone levels. The difference between function and goiter size with respect to thyroid stimulating antibody measurement in two cells system is, nevertheless, particularly evident in the free T4/goiter ratio in patients with high hTSHR-CHO and low FRTL-5 cell assay values. Conclusion: These findings suggest that thyroid stimulating antibodies in Graves disease are heterogeneous population in terms of responses to different origin of cells. Further, thyroid stimulating antibody activities measured by FRTL-5 cells tend to correlate better with goiter size and Tc-thyroid uptake, whereas thyroid stimulating antibody activities measured by hTSH-CHO cells correlate better with thyroid hormone levels.


 KES
KES

 First
First Prev
Prev



